Overview
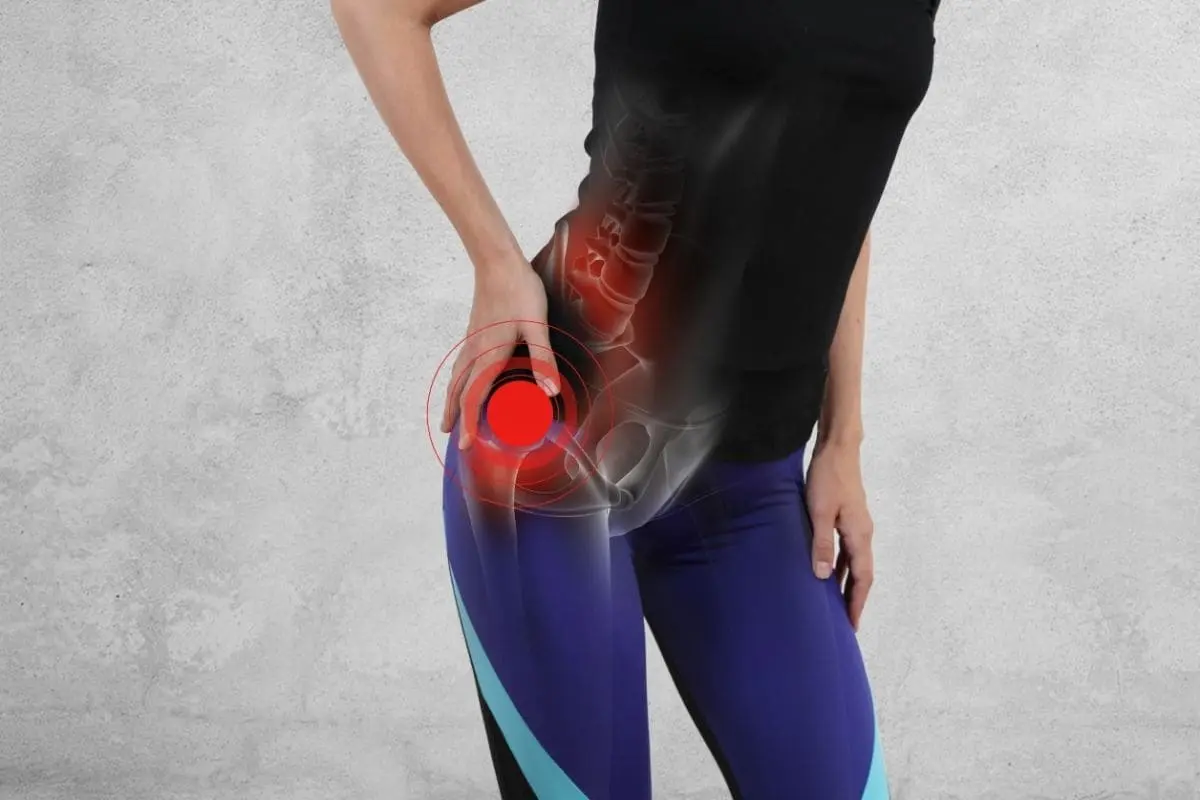
Gluteus minimus tendinitis is a painful condition characterized by inflammation or degeneration of the gluteus minimus tendon, one of the key stabilizing tendons of the hip joint. The gluteus minimus, a small but powerful muscle located deep in the lateral hip region beneath the gluteus medius, plays a vital role in hip abduction, pelvic stability, and walking mechanics.
When this tendon becomes irritated or inflamed due to overuse, trauma, or biomechanical imbalances, it results in gluteus minimus tendinitis, a condition often mistaken for greater trochanteric pain syndrome or bursitis. The pain typically radiates from the outer hip region down the lateral thigh, mimicking sciatica or hip arthritis, making accurate diagnosis essential.
At DMPhysios, a leading clinic in Noida specializing in spine and sports conditions with patient-centered rehabilitation, experts emphasize a holistic and evidence-based approach to managing gluteus minimus tendinitis, focusing on restoring function, relieving pain, and preventing recurrence.
Symptoms
The symptoms of gluteus minimus tendinitis can range from mild discomfort to severe pain that interferes with daily activities. Key clinical features include:
- Lateral Hip Pain:
A deep, aching pain on the outer side of the hip, often radiating down the outer thigh toward the knee. The pain may worsen when lying on the affected side, standing on one leg, or climbing stairs. - Tenderness at the Greater Trochanter:
Pain and tenderness when pressing on the bony prominence on the outer hip (greater trochanter) are common signs. - Difficulty in Walking or Standing:
Prolonged walking, running, or even standing can aggravate the discomfort due to constant activation of the gluteus minimus tendon. - Weakness in Hip Abduction:
Reduced strength when moving the leg away from the body (abduction) indicates gluteal tendon involvement. - Pain during Side-Lying Sleeping:
Sleeping on the affected side increases compression on the tendon, worsening pain at night. - Referred Pain:
Pain may extend to the outer thigh or buttock region, occasionally mistaken for lumbar or sciatic pain.
Recognizing these symptoms early and seeking expert evaluation at DMPhysios can prevent chronic degeneration and promote faster recovery from gluteus minimus tendinitis.
Types of Gluteus Minimus Tendinitis
Though not officially classified into multiple types, gluteus minimus tendinitis can be categorized based on the underlying pathology and stage of injury:
- Acute Gluteus Minimus Tendinitis:
Inflammation due to sudden strain, trauma, or overuse, often presenting with swelling and localized tenderness. - Chronic Degenerative Tendinopathy:
Long-standing tendon wear without active inflammation, involving microtears, collagen disorganization, and weakening of the tendon structure. - Partial or Full-Thickness Tears:
In severe or neglected cases, the inflamed tendon may partially or fully tear, requiring a longer rehabilitation period or even surgical consultation.
Causes
Multiple intrinsic and extrinsic factors contribute to gluteus minimus tendinitis. The most common causes include:
- Overuse and Repetitive Stress:
Repeated hip movements in athletes, dancers, or runners can overload the tendon, causing irritation. - Poor Biomechanics:
Abnormal gait patterns, leg length discrepancies, or weak core muscles lead to excessive hip strain. - Sudden Trauma:
A direct fall on the hip or sudden twisting movement can inflame or strain the gluteus minimus tendon. - Muscle Imbalance:
Weak gluteal muscles coupled with tight hip flexors or adductors increase tendon stress. - Aging and Degeneration:
Reduced blood supply and collagen degeneration in older adults can predispose to tendinopathy. - Improper Training Technique:
Incorrect posture or poor warm-up before sports or gym workouts can trigger gluteus minimus tendinitis. - Prolonged Sitting or Pressure:
Continuous sitting compresses the lateral hip muscles, reducing circulation and increasing stiffness.
At DMPhysios, expert physiotherapists perform a detailed biomechanical assessment to identify the root cause and design personalized treatment for gluteus minimus tendinitis.
Risk Factors
Certain individuals are more prone to developing gluteus minimus tendinitis, including:
- Middle-aged and older adults (especially women)
- Runners, cyclists, and long-distance walkers
- Individuals with poor posture or weak gluteal muscles
- People with hip osteoarthritis or spinal dysfunction
- Those recovering from lower limb injuries or surgeries
- Obesity, which increases load on the hip joint
Understanding these risk factors allows the physiotherapy team at DMPhysios, Noida, to implement preventive measures and reduce recurrence.
Treatment
Effective management of gluteus minimus tendinitis involves addressing inflammation, relieving pain, restoring muscle balance, and improving functional mobility.
1. Medical Management
- Rest and Activity Modification: Avoid painful activities like prolonged standing, stair climbing, or side-lying on the affected side.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Used to reduce pain and inflammation under medical supervision.
- Cold and Heat Therapy: Ice application in the acute phase and heat in later stages aid in pain relief and tissue healing.
- Corticosteroid Injections: In some cases, local injections near the greater trochanter may be prescribed for severe inflammation.
- Shockwave Therapy or PRP: Advanced treatments that stimulate tendon healing and regeneration.
However, physiotherapy remains the cornerstone of long-term recovery and prevention of recurrence in gluteus minimus tendinitis, and this is where DMPhysios excels.
Physiotherapy Treatment
At DMPhysios, a clinic in Noida renowned for its expertise in spine and sports rehabilitation, physiotherapists provide an evidence-based, patient-centered rehabilitation plan for gluteus minimus tendinitis. The approach focuses on relieving pain, restoring strength, correcting biomechanics, and preventing future flare-ups.
1. Pain Management Techniques
- Ultrasound Therapy: Promotes deep tissue healing and reduces inflammation around the gluteus minimus tendon.
- Accelerated Healing Therapy: Enhances cellular recovery and reduces chronic pain.
- Cryotherapy: Cold therapy used during acute stages to decrease inflammation.
- TENS (Transcutaneous Electrical Nerve Stimulation): Helps modulate pain signals and improve comfort.
2. Manual Therapy
Hands-on therapy is a crucial part of the rehabilitation process at DMPhysios:
- Soft Tissue Mobilization: Reduces adhesions and muscle tightness in the gluteal and iliotibial (IT) band region.
- Myofascial Release: Releases deep muscle restrictions improving mobility.
- Joint Mobilization: Enhances hip joint range of motion and reduces mechanical stress on the tendon.
3. Stretching Exercises
Stretching helps in relieving tension and restoring normal length-tension balance:
- Gluteus minimus stretch
- Piriformis stretch
- Hip flexor stretch
- Tensor fasciae latae (TFL) stretch
4. Strengthening Exercises
Strengthening is a key phase in rehabilitation at DMPhysios:
- Isometric Hip Abduction: Initiated early to engage the gluteus minimus safely.
- Clamshell Exercise: Strengthens gluteus minimus and medius effectively.
- Side-lying Leg Raises: Builds lateral hip strength without joint strain.
- Bridging Variations: Improves pelvic stability and gluteal activation.
- Single-leg Balance Training: Restores neuromuscular control and coordination.
5. Functional and Corrective Training
Physiotherapists at DMPhysios incorporate gait retraining, posture correction, and functional strengthening:
- Gait Re-education: Corrects compensatory movement patterns.
- Core Strengthening: Enhances overall stability and reduces hip load.
- Return-to-Sport Drills: Gradually reintroduces sports-specific activities for athletes recovering from gluteus minimus tendinitis.
6. Education and Ergonomic Advice
Patients are educated on proper sitting, sleeping positions, and ergonomics to minimize tendon strain during daily life.
Prevention
Preventing gluteus minimus tendinitis involves maintaining healthy movement mechanics and muscle balance. Follow these preventive strategies recommended by DMPhysios experts:
- Warm-up and Cool-down:
Always prepare the muscles before activity and stretch afterward. - Strengthen Gluteal and Core Muscles:
Maintain hip and pelvic stability through regular strengthening exercises. - Avoid Overtraining:
Gradually increase workout intensity and duration. - Maintain Proper Posture:
Avoid slouching or leaning to one side when sitting or standing. - Use Supportive Footwear:
Proper shoes with good arch support reduce abnormal hip stress. - Ergonomic Modifications:
Adjust seating height and avoid prolonged sitting on hard surfaces. - Early Physiotherapy Intervention:
At the first sign of hip discomfort, consulting the specialists at DMPhysios helps prevent progression to chronic tendinopathy.
Conclusion
Gluteus minimus tendinitis may seem like a minor soft tissue problem, but if left untreated, it can lead to chronic hip pain and reduced mobility, affecting overall quality of life. Accurate diagnosis, proper rehabilitation, and biomechanical correction are vital for complete recovery.
At DMPhysios, Noida’s trusted center for spine and sports conditions, the physiotherapy team uses a patient-centered approach that combines manual therapy, advanced modalities, and customized exercise programs to ensure optimal recovery from gluteus minimus tendinitis.
If you are struggling with persistent hip pain, discomfort while walking, or difficulty lying on one side, don’t ignore the symptoms. Visit DMPhysios today to receive a personalized assessment and begin your journey toward a pain-free, active lifestyle.
Your recovery starts with movement, let DMPhysios help you move better, live stronger, and stay pain-free.