Overview
Lumbar myelopathy is a serious neurological disorder that arises when there is compression, irritation, or damage to the spinal cord structures in the lumbar region of the spine. Although the spinal cord typically ends around the upper lumbar levels, conditions affecting the conus medullaris or nearby neural elements can still produce symptoms consistent with myelopathy. This makes lumbar myelopathy less common than cervical myelopathy, yet equally important to diagnose and treat promptly.
The condition can lead to a wide range of neurological impairments. Many individuals experience a gradual decline in lower limb strength, altered sensation, and reduced motor control. In more advanced cases, walking becomes increasingly difficult, balance is compromised, and bladder or bowel function may be affected—leading to a significant impact on independence and quality of life.
Functionally, the spinal cord serves as the main communication link between the brain and the rest of the body, transmitting both movement commands and sensory feedback. In lumbar myelopathy, this information flow is disrupted, often due to structural degeneration, traumatic injury, inflammatory disorders, tumors, or other space-occupying lesions. Such disruption, if left untreated, can cause irreversible nerve damage and long-term disability.
At DMPhysios, a premier physiotherapy clinic based in Noida with expertise in spine and sports rehabilitation, the approach to lumbar myelopathy is highly patient-centered. Each individual undergoes a comprehensive evaluation, after which a tailored, evidence-based rehabilitation program is designed. The goal is not only to relieve symptoms but also to restore functional mobility, enhance daily performance, and help patients regain confidence in their physical abilities.
Symptoms
The symptoms of lumbar myelopathy often develop gradually, but in some cases, they may progress rapidly depending on the cause. Common symptoms include:
- Lower limb weakness – Difficulty lifting the feet, reduced walking speed, or frequent tripping.
- Numbness or tingling – Often in the legs, feet, or perineal region.
- Balance problems – A shuffling gait or difficulty maintaining stability.
- Loss of fine motor control – Reduced ability to perform precise leg or foot movements.
- Bladder and bowel dysfunction – Urgency, frequency, incontinence, or retention.
- Pain – Aching or burning sensation in the lower back or legs.
- Spasticity or stiffness – Involuntary muscle tightness in the lower extremities.
Recognizing these symptoms early is critical. Patients who seek assessment at DMPhysios benefit from comprehensive neurological evaluation and functional testing to detect even subtle deficits.
Types of Lumbar Myelopathy
Although lumbar myelopathy is far less common than its cervical counterpart, it can manifest in several distinct forms depending on the nature and origin of the underlying problem. Identifying the specific type is essential, as it directly influences the treatment plan and expected recovery outcomes.
- Degenerative Lumbar Myelopathy – This is the most frequently encountered form in older adults and is caused by age-related changes in the spine. Conditions such as lumbar spondylosis, degenerative disc disease, or thickening of spinal ligaments can gradually narrow the spinal canal, placing pressure on the spinal cord or nerve roots in the lumbar region. The progression is often slow but can steadily impair mobility and function if not addressed.
- Traumatic Lumbar Myelopathy – This type results from sudden, forceful injury to the lower spine, such as fractures, dislocations, or direct trauma to the spinal cord. Road accidents, high-impact sports, or falls from height are common causes. The damage may occur instantly and can lead to immediate and severe neurological deficits, often requiring urgent medical and rehabilitative intervention.
- Tumor-related Lumbar Myelopathy – Both benign and malignant growths in or around the lumbar spine can compress the spinal cord. Primary spinal tumors may originate within the cord or surrounding structures, while secondary (metastatic) tumors spread from cancers elsewhere in the body. Tumor-related compression often progresses gradually but may be accompanied by persistent pain, weakness, or other warning signs.
- Inflammatory or Infectious Lumbar Myelopathy – Conditions such as transverse myelitis, autoimmune disorders, or spinal infections like tuberculosis can inflame or damage spinal cord tissue in the lumbar region. These cases may have a rapid onset and often require both medical management of the underlying disease and focused rehabilitation to restore function.
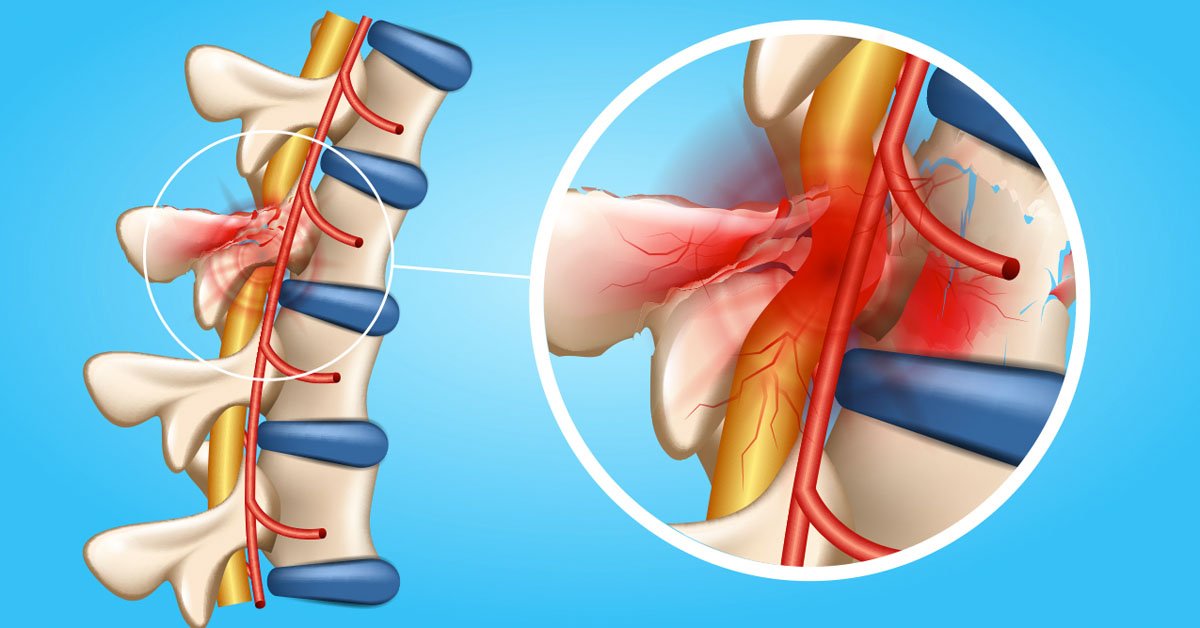
- Vascular Lumbar Myelopathy – Reduced blood flow to the spinal cord—such as from a spinal cord infarction, vascular malformations, or blood clots—can deprive the neural tissue of oxygen and nutrients. This type may develop suddenly and can result in irreversible injury if circulation is not restored promptly.
Recognizing the exact category of lumbar myelopathy is the first step toward an effective care strategy. At DMPhysios, a specialized spine and sports rehabilitation clinic in Noida, the team carefully evaluates the cause, severity, and progression of the condition before designing a personalized rehabilitation plan. This ensures that treatment is not only targeted but also optimizes recovery potential for each patient.
Causes
Several conditions can cause lumbar myelopathy, including:
- Lumbar spinal stenosis – Narrowing of the spinal canal due to bone overgrowth, ligament thickening, or disc bulges.
- Disc herniation – Protrusion of the intervertebral disc pressing on the spinal cord.
- Spinal cord tumors – Both primary and metastatic lesions.
- Trauma – Falls, road accidents, or sports injuries.
- Inflammatory diseases – Multiple sclerosis, autoimmune disorders, or infections.
- Congenital spinal abnormalities – Spina bifida or tethered cord syndrome.
- Vascular disorders – Blood clots, arteriovenous malformations, or ischemia.
Risk Factors
Certain factors increase the risk of developing lumbar myelopathy:
- Age – Degenerative changes become more common after age 50.
- History of spinal injury – Prior trauma increases vulnerability.
- Genetic predisposition – Some individuals inherit structural spine abnormalities.
- Occupation – Jobs involving heavy lifting or prolonged sitting.
- Chronic inflammatory conditions – Autoimmune or infectious spinal diseases.
- Tumors or cancer history – Especially cancers that metastasize to the spine.
- Obesity – Increased load on the spine accelerates degeneration.
Treatment
The treatment approach depends on the severity, cause, and progression of symptoms. Options include:
- Medications
- Anti-inflammatory drugs to reduce swelling and pain.
- Muscle relaxants for spasticity.
- Neuropathic pain medications.
- Surgical intervention
- Decompression surgery for spinal stenosis.
- Tumor removal when applicable.
- Spinal fusion for instability.
- Rehabilitation
- Physiotherapy for restoring strength, mobility, and coordination.
- Occupational therapy for adapting daily activities.
- Lifestyle modifications
- Weight management.
- Ergonomic adjustments at work and home.
At DMPhysios, post-surgical rehabilitation for lumbar myelopathy is highly specialized, aiming to accelerate recovery and restore optimal function.
Physiotherapy Treatment
Physiotherapy plays a central role in managing lumbar myelopathy, both in conservative treatment and post-surgical recovery. At DMPhysios, the rehabilitation program is designed to address muscle weakness, mobility deficits, and balance impairments while considering the patient’s specific neurological limitations.
1. Initial Assessment
- Neurological examination (strength, reflexes, sensation).
- Gait and posture analysis.
- Functional mobility testing (sit-to-stand, timed walking tests).
2. Pain and Inflammation Management
- Electrotherapy – Accelerated Healing Therapy for better and fast healing.
- Cryotherapy or thermotherapy – Depending on symptom stage.
3. Strengthening Exercises
- Core stability training – Transverse abdominis and multifidus activation to support spinal stability.
- Lower limb strengthening – Quadriceps, hamstrings, glutes, and calf muscles.
- Progressive resistance exercises – Using bands or light weights.
4. Flexibility and Mobility Training
- Passive and active range-of-motion exercises for hips, knees, and ankles.
- Gentle lumbar spine mobilization to maintain joint nutrition and flexibility.
5. Balance and Coordination Exercises
- Static balance drills (single-leg stance, tandem stance).
- Dynamic balance tasks (step-ups, weight shifts).
- Use of unstable surfaces (foam pads, balance boards) for proprioception training.
6. Gait Retraining
- Cueing for proper foot placement.
- Treadmill walking with or without body-weight support.
- Assistive device training (canes, walkers) if needed.
7. Functional Training
- Practicing sit-to-stand, stair climbing, and bed mobility.
- Task-specific activities to restore independence in daily life.
8. Postural Education
- Ergonomic corrections for sitting, standing, and lifting.
- Education on safe body mechanics to prevent further injury.
9. Home Exercise Program
- Customized exercise routines to maintain progress outside clinic sessions.
- Regular follow-up to adjust intensity and complexity.
At DMPhysios, therapy sessions are patient-focused, progressive, and evidence-based, ensuring that individuals with lumbar myelopathy regain maximum independence.
Prevention
While not all cases can be prevented, the following measures may reduce the risk of lumbar myelopathy:
- Maintain a healthy weight to reduce spinal stress.
- Engage in regular core-strengthening and flexibility exercises.
- Avoid prolonged poor posture, especially during desk work.
- Use correct lifting techniques to protect the spine.
- Treat spinal injuries promptly.
- Manage chronic diseases like diabetes and arthritis effectively.
- Undergo routine spine health check-ups, especially if in a high-risk group.
Conclusion
Lumbar myelopathy is a serious spinal cord condition that can lead to significant disability if left untreated. However, with early diagnosis, targeted treatment, and comprehensive rehabilitation, many patients can recover function and maintain an active lifestyle.
At DMPhysios, located in Noida and specializing in spine and sports conditions, the approach to managing lumbar myelopathy is patient-centered, combining advanced physiotherapy techniques, clinical expertise, and individualized care plans. Whether you require conservative management or post-surgical rehab, the team at DMPhysios is dedicated to helping you restore mobility, independence, and quality of life.
If you or a loved one is experiencing symptoms of lumbar myelopathy, don’t wait for them to worsen—schedule a consultation with DMPhysios today and take the first step toward recovery.