Overview
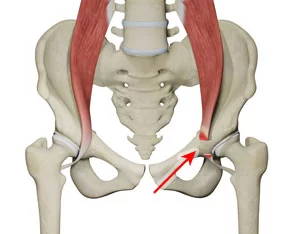
Iliopsoas tendinitis is considered an overuse injury that specifically affects the iliopsoas tendon, which is formed by the confluence of two powerful muscles, the psoas major and the iliacus. Together, these muscles are primarily responsible for hip flexion, enabling everyday actions like walking, climbing stairs, and running. They also play an essential role in stabilizing the pelvis and maintaining upright posture. Because of the constant demands placed on these muscles and their tendon, repetitive strain or sudden overload can lead to irritation and inflammation of the iliopsoas tendon, resulting in pain, stiffness, and difficulty with movement.
What makes iliopsoas tendinitis particularly challenging is that its clinical presentation often overlaps with other hip-related conditions. Patients may present with groin pain or hip discomfort that resembles hip labral tears, femoroacetabular impingement (FAI), or iliopsoas bursitis. This overlap can delay accurate diagnosis and treatment, leading to persistent symptoms if not carefully evaluated. In fact, iliopsoas tendinitis is often underdiagnosed in both athletes and non-athletes because the pain may be vague or attributed to other common musculoskeletal issues.
Early recognition is vital, as untreated iliopsoas tendinitis can progress into chronic pain and reduced hip function, limiting not only sports performance but also basic daily activities. Comprehensive care that combines accurate diagnosis, medical management, and progressive rehabilitation ensures the best outcomes. Clinics that specialize in spine and sports conditions, such as DMPhysios in Noida, are particularly well-equipped to handle such cases. Their approach is centered around patient-focused rehabilitation, which means identifying the underlying biomechanical causes of the condition and tailoring a recovery plan that not only addresses current pain but also prevents recurrence.
Symptoms
The clinical presentation of iliopsoas tendinitis often varies depending on the severity of inflammation and the level of activity. Common symptoms include:
- Pain in the anterior hip or groin region, especially during hip flexion activities.
- Discomfort when climbing stairs, walking uphill, or transitioning from sitting to standing.
- A snapping or clicking sensation in the front of the hip (sometimes referred to as “internal snapping hip”).
- Tenderness upon palpation of the iliopsoas tendon.
- Stiffness or tightness in the hip flexors.
- Pain that may radiate toward the thigh or lower back in more severe cases.
In athletes or individuals with high activity levels, pain may worsen after prolonged running, kicking, or repetitive hip flexion activities.
Types of Iliopsoas Tendinitis
1. Acute Iliopsoas Tendinitis
- Sudden onset of pain due to overuse or acute strain.
- Common in athletes who perform repetitive hip flexion (runners, footballers, martial artists).
- Symptoms: sharp anterior hip or groin pain, often after intense activity.
2. Chronic Iliopsoas Tendinitis
- Develops gradually from long-term irritation and repetitive movements.
- Linked to poor biomechanics, weak glutes/core, or prolonged sitting.
- Symptoms: dull, persistent ache that worsens with activity and improves temporarily with rest.
3. Iliopsoas Tendinitis with Bursitis
- Inflammation of the iliopsoas tendon occurs alongside irritation of the iliopsoas bursa.
- Leads to more severe pain, snapping or clicking sensation in the hip, and difficulty extending the leg fully.
- Often requires a combination of medical management and physiotherapy.
Causes
Several factors contribute to the development of iliopsoas tendinitis. These include:
- Overuse: Repetitive hip flexion in activities such as running, cycling, or soccer.
- Biomechanical abnormalities: Poor posture, pelvic instability, or improper gait patterns.
- Muscle imbalances: Weak gluteal or core muscles leading to overcompensation by the iliopsoas.
- Sudden increases in training load: Rapid escalation in workout intensity without adequate conditioning.
- Trauma: Direct injury or overstretching of the hip flexors.
- Hip joint dysfunction: Underlying conditions such as femoroacetabular impingement can increase tendon stress.
Risk Factors
Not everyone develops iliopsoas tendinitis, but certain populations are more vulnerable:
- Athletes: Particularly runners, footballers, dancers, and martial artists.
- Individuals with weak core stability: Poor lumbopelvic control increases stress on the hip flexors.
- People with sedentary lifestyles: Prolonged sitting leads to hip flexor tightness, predisposing tendons to injury once activity is resumed.
- Older adults: Age-related tendon degeneration makes tendons more prone to inflammation.
- Post-surgical patients: Hip or spine surgeries may alter movement mechanics, increasing strain on the iliopsoas tendon.
Treatment
The management of iliopsoas tendinitis requires a combination of rest, medical intervention, and structured rehabilitation. Common treatment approaches include:
- Rest and activity modification: Reducing aggravating movements such as running or uphill climbing.
- Ice therapy: Applying ice packs to reduce acute inflammation.
- Anti-inflammatory medications: NSAIDs prescribed for pain relief and inflammation control.
- Injections: Corticosteroid injections into the tendon or bursa in resistant cases.
- Manual therapy: Soft tissue mobilization to reduce tension and improve circulation.
- Gradual return to activity: Once pain subsides, patients should follow a structured rehabilitation program.
At DMPhysios in Noida, a comprehensive assessment is carried out to identify both the cause and the contributing biomechanical issues, ensuring that treatment is not just about symptom relief but also long-term prevention.
Physiotherapy Treatment
Physiotherapy plays the most crucial role in managing iliopsoas tendinitis. A structured program helps reduce pain, restore mobility, and prevent recurrence.
1. Pain Relief Techniques
- Ultrasound therapy and interferential therapy for reducing tendon irritation.
- Soft tissue release techniques on the iliopsoas and surrounding hip flexors.
- IASTM (Instrument-Assisted Soft Tissue Mobilization) for improving tissue mobility.
2. Stretching Exercises
- Iliopsoas stretch (lunge stretch): Helps release tension in the hip flexors.
- Quadriceps and hamstring stretches: To balance muscle groups around the hip.
- Piriformis stretch: To reduce compensatory tightness in hip stabilizers.
3. Strengthening Exercises
Strengthening the surrounding musculature is critical for long-term recovery.
- Glute bridges: Target gluteal activation to reduce reliance on hip flexors.
- Clamshells: Improve hip abductor strength.
- Core stabilization exercises: Planks, side planks, and dead bugs to support pelvic stability.
- Progressive resisted hip flexion: Controlled strengthening once inflammation reduces.
4. Functional Training
- Gait retraining to correct movement mechanics.
- Sports-specific drills for athletes to gradually reintroduce activity.
5. Postural and Ergonomic Education
Patients are educated on sitting posture, standing alignment, and movement strategies to prevent recurrence.
At DMPhysios, the physiotherapy team emphasizes patient-centered rehabilitation, meaning each treatment plan is customized to the individual’s needs, lifestyle, and goals. This ensures not only recovery from iliopsoas tendinitis but also resilience against future injuries.
Prevention
Preventive strategies are as important as treatment in managing iliopsoas tendinitis:
- Regular stretching of hip flexors and surrounding muscles.
- Strengthening of glutes and core muscles to reduce load on the iliopsoas tendon.
- Gradual progression in training to avoid sudden overload.
- Proper warm-up and cool-down routines before and after exercise.
- Maintaining good posture while sitting, standing, and walking.
- Correct footwear to reduce biomechanical stress during activity.
By incorporating these preventive strategies, individuals, especially athletes can minimize the chances of recurring tendon problems. Clinics like DMPhysios in Noida guide patients through preventive conditioning and post-rehabilitation follow-ups.
Conclusion
Iliopsoas tendinitis is a painful yet manageable condition that significantly impacts mobility and quality of life if left untreated. Recognizing its symptoms early, addressing the root causes, and undergoing a structured physiotherapy program are key steps toward recovery.
At DMPhysios in Noida, patients receive a comprehensive, patient-centered rehabilitation approach that focuses not only on pain relief but also on restoring full functional capacity and preventing recurrence. If you or someone you know is experiencing hip or groin pain suggestive of iliopsoas tendinitis, timely intervention can make all the difference.
Take the first step today, reach out to DMPhysios for expert care and a tailored rehabilitation program that helps you return to an active, pain-free lifestyle.