Baxter’s neuropathy, also referred to as inferior calcaneal nerve entrapment or first branch of the lateral plantar nerve entrapment, is a condition in which the small but important nerve that runs along the inner heel – the inferior calcaneal nerve (commonly called Baxter’s nerve) – becomes compressed, irritated or trapped between surrounding soft-tissue or bony structures. This entrapment can interfere with the normal transmission of sensory and motor signals, leading to a combination of pain, altered sensation, weakness and in some cases muscle wasting in the foot.
Although not as widely recognised as plantar fasciitis or heel spurs, Baxter’s neuropathy is now understood to be one of the major, yet underdiagnosed, causes of persistent or recurrent heel pain. Patients often present with discomfort along the medial or underside of the heel, sometimes with a burning or tingling quality, and the symptoms are frequently mislabelled as plantar fasciitis because of their overlap. If the nerve compression is left untreated, the ongoing irritation can contribute to changes in gait, reduced push-off power, and atrophy of the small muscles of the foot, ultimately limiting mobility and quality of life.
At DMPhysios, a leading Noida-based clinic specialising in spine and sports conditions with a strong emphasis on patient-centred rehabilitation, recognising and differentiating Baxter’s neuropathy from more common heel pathologies is a critical part of our approach. Early and accurate diagnosis allows the team to design targeted treatment plans that relieve pressure on the nerve, restore function, and help patients return to their normal activities without chronic pain. By understanding the unique anatomy and mechanics of Baxter’s nerve, DMPhysios clinicians ensure that this often-overlooked source of heel pain does not remain undetected or mismanaged.
Symptoms
The presentation of Baxter’s neuropathy may vary, but common symptoms include:
- Heel pain, particularly medial heel pain, often worse when standing, walking, or first thing in the morning.
- Pain along the course of inferior calcaneal nerve: in the plantar medial aspect of the heel and anterior to the medial aspect of the calcaneus.
- Paresthesia: tingling, “pins and needles,” burning sensation in the heel, sometimes extending partly into the arch.
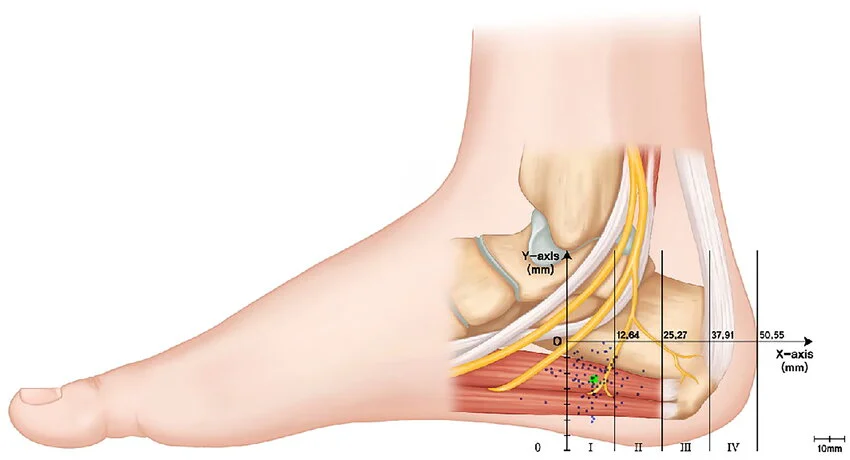
- Local tenderness when pressing over the path of Baxter’s nerve, for example near the medial calcaneal tuberosity, or along the abductor hallucis or quadratus plantae.
- Weakness or atrophy of muscles innervated by Baxter’s nerve (notably abductor digiti minimi muscle of the foot). In some cases, selective fatty atrophy of abductor digiti minimi muscle is visible on imaging.
- Pain may worsen with activity, especially walking or running, and often relieved by rest.
- Sometimes symptoms mimic plantar fasciitis (because of the overlap or co-existence). Indeed, Baxter’s neuropathy may follow or be secondary to plantar fasciitis.
Types of Baxter’s Neuropathy
Baxter’s neuropathy is fairly specific (i.e. entrapment of Baxter’s nerve), so it doesn’t have “types” in the way peripheral neuropathy broadly does (e.g. diabetic, toxic). However, there are distinctions and associations:
- Primary Baxter’s neuropathy: where the nerve entrapment arises without other obvious pathology (e.g. due to anatomical variants, muscle hypertrophy).
- Secondary Baxter’s neuropathy: occurs as a complication of other foot pathologies like plantar fasciitis, heel spurs (plantar calcaneal enthesophytes), or altered foot biomechanics (flatfoot, overpronation).
- Acute vs chronic: symptoms may start acutely (after overuse, trauma) or develop slowly over time.
- Unilateral vs bilateral: while often one foot is affected, there are reports of bilateral Baxter’s neuropathy (e.g. in bilateral plantar fasciitis)
Differential diagnoses to consider when suspecting Baxter’s neuropathy:
- Plantar fasciitis
- Tarsal tunnel syndrome
- Heel spur pain
- Other entrapment neuropathies of tibial / lateral plantar nerve
- Stress fractures or other bony pathologies
- Overuse injuries of soft tissues
Causes
The causes of Baxter’s neuropathy are generally related to mechanical compression, anatomical factors or associated pathologies. Key causes include:
- Entrapment by muscles
- Hypertrophy of abductor hallucis muscle, impinging on the nerve.
- The medial edge of the quadratus plantae muscle.
- Bony factors / structural changes
- Plantar calcaneal spur (heel spur) causing irritation/compression.
- Medial calcaneal tuberosity growth or deformity.
- Associated pathologies
- Plantar fasciitis is one of the most common associated diagnoses, and in some cases Baxter’s neuropathy arises secondary to plantar fasciitis.
- Achilles tendinosis or other alterations in foot biomechanics.
- Biomechanical abnormalities
- Flatfoot (pes planus), overpronation, or altered arch shape which increases tension/compression of the nerve.
- Increased weight, obesity, or overload of the feet.
- Trauma or repeated micro trauma
- Repetitive stress from running, jumping, or walking on uneven surfaces.
- Direct heel injury.
- Other risk factors (see next section) that may exacerbate or predispose to the development of Baxter’s neuropathy.
Risk Factors
Some individuals are more likely to develop Baxter’s neuropathy due to the following risk factors:
- Foot biomechanics issues: flat feet, overpronation, high arches, or deformity that causes abnormal stress.
- Repeated or prolonged load bearing activities: runners, athletes, people standing long hours, or those engaged in sports with frequent jumping or direction changes.
- Excessive weight / obesity, increasing load through the heel.
- Age: with time there can be degenerative changes in foot soft tissue, muscle, or fascia that can contribute.
- Footwear: poorly supportive shoes, thin soles, or shoes that irritate/press the heel area.
- Co-existing conditions: plantar fasciitis, heel spurs, tendinopathies, prior foot injury.
- Occupation: jobs that involve standing, walking on hard surfaces, frequent load, etc.
- Delay in diagnosis or treatment which allows the condition to become chronic (leading to muscle atrophy)
Treatment
Management of Baxter’s neuropathy generally starts with conservative (non-surgical) methods; surgery is considered when conservative measures fail. Key treatment strategies include:
- Rest and activity modification
- Reducing weight-bearing activities, avoiding prolonged standing or repetitive shock to the heel.
- Modifying sports/training until symptoms reduce.
- Footwear adjustments
- Wearing shoes with good arch support, cushioning in the heel, firm heel counter.
- Use of orthotics (custom or prefabricated) to correct overpronation or redistribute load.
- Medication / Pharmacological care
- NSAIDs for pain and inflammation relief.
- Occasionally neuropathic pain medications if nerve pain severe, under clinical supervision.
- Ice and modalities
- Application of ice to reduce inflammation.
- Use of physical therapy modalities: ultrasound, shock wave therapy, laser, etc.
- Injection therapy
- Corticosteroid injections near the entrapped nerve or into the plantar fascia if associated with plantar fasciitis.
- Sometimes local anaesthetic blocks.
- Surgical intervention
- Decompression of Baxter’s nerve if all conservative measures fail.
- Release of fascia, removal of spurs, and other structures causing entrapment.
- Outcomes are generally good, but surgery carries risks, recovery time.
Physiotherapy Treatment
At DMPhysios in Noida, with its patient-centred rehabilitation model, physiotherapy plays a vital role in the management of Baxter’s neuropathy. Following is a detailed physiotherapy treatment plan.
Assessment
- Thorough clinical evaluation: history of the heel pain, duration, aggravating/relieving factors, gait analysis.
- Physical examination: palpation over medial heel, calcaneal tuberosity, abductor hallucis muscles; testing for muscle weakness, atrophy (especially abductor digiti minimi), checking arch height, foot alignment.
- Diagnostic imaging: MRI may reveal fatty atrophy of muscles, plantar fasciitis, heel spurs; ultrasound may help in detecting nerve swelling or entrapment.
- Functional assessment: walking, standing, imbalance, footwear analysis.
Treatment Phases
- Acute Phase (Pain Relief & Inflammation Control)
- Patronised rest: reduce load, avoid activities that worsen pain.
- Manual therapy: soft tissue massage around abductor hallucis, plantar fascia, calf muscles to reduce tension.
- Stretching: gentle stretching of plantar fascia, Achilles tendon, calves.
- Modalities: therapeutic ultrasound, ice massage, laser therapy to reduce inflammation and pain.
- Neural mobilisation: gentle mobilisations of the Baxter nerve if possible, nerve gliding techniques (with care).
- Rehabilitative Phase (Strengthening & Restoration of Function)
- Muscle strengthening: especially intrinsic foot muscles (abductor hallucis, abductor digiti minimi), calf muscles. Exercises like toe spread, towel scrunch, toe abduction/adduction, heel raises.
- Proprioceptive training / balance exercises: wobble board, single leg stance, walking on uneven surfaces (gradually).
- Gait training: correcting patterns, ensuring heel strike-midfoot-toe off phases are correct, avoiding overpronation.
- Correction of Biomechanics / Orthotic Support
- Use of off-the-shelf or custom orthotics or insoles to support arch, reduce overpronation, cushion heel.
- Footwear education: proper soles, heel pads, cushioning, avoiding flat or unsupportive shoes.
- Advanced & Maintenance Phase
- Gradual return to sports or high load activity with progressive loading.
- Plyometric or sport-specific drills, once pain-free movement is achieved.
- Education: on prevention strategies, recognizing flare ups, self-care of feet.
- Adjunctive Therapies
- Shock wave therapy may be used in cases associated with plantar fasciitis.
- Ultrasound guided hydrodissection is being reported in some literature for Baxter’s neuropathy secondary to plantar fasciitis.
- Other modalities: electrical stimulation, nerve repair therapies if applicable.
Expected Outcomes & Monitoring
- Improvement in pain, decreased paresthesia, improved muscle strength (especially abductor digiti minimi), less tenderness.
- Monitoring via functional scales, pain Visual Analog Scale, gait assessment.
- If after a defined period (usually several weeks to months) of conservative treatment there is no improvement, consider imaging, specialist referral, possibly surgical decompression.
At DMPhysios, the patient-centred rehab approach means therapy plans are individualized, progression is monitored closely, and patients are involved in goal setting.
Prevention
Preventing Baxter’s neuropathy (or preventing it from worsening) involves several proactive measures:
- Appropriate footwear: use supportive shoes, avoid shoes with little cushioning or poor arch support. Replace worn shoes.
- Maintain healthy weight: reduces load on foot structures.
- Warm up and stretching: especially for runners or athletes. Stretch calves, plantar fascia, Arch.
- Avoid overuse: gradually increase activity levels; cross-training to reduce repetitive strain.
- Biomechanical check: if overpronation or other foot alignment issues, use orthotics or arch supports early.
- Manage associated conditions: treat plantar fasciitis early; ensure tight muscles (calves, plantar fascia) don’t continue to pull and compress.
- Regular foot care: massage, foot strengthening, ensure no “hot spots,” pain early and resting.
Conclusion
In summary, Baxter’s neuropathy is a not-so-rare contributor to heel pain that often masquerades as plantar fasciitis or similar foot problems. The key lies in early diagnosis, correct identification of the entrapment of the inferior calcaneal (Baxter’s) nerve, and timely, patient-centred treatment. Conservative management via rest, footwear, orthotics, manual therapy, neural mobilisation, and targeted strengthening often gives very good results. In recalcitrant cases, surgical decompression may be needed.
If you are experiencing persistent heel pain, tingling, or weakness in the foot, think of Baxter’s neuropathy as one possible cause. DMPhysios, in Noida, with its focus on spine and sports conditions and patient-centred rehab, is well equipped to assess, diagnose and manage Baxter’s neuropathy. Don’t wait for months with discomfort; early intervention means faster recovery, less risk of chronic changes and better functional outcome. Contact DMPhysios today to schedule a consultation, assessment, and personalised rehabilitation plan to get you back to pain-free movement.