Overview
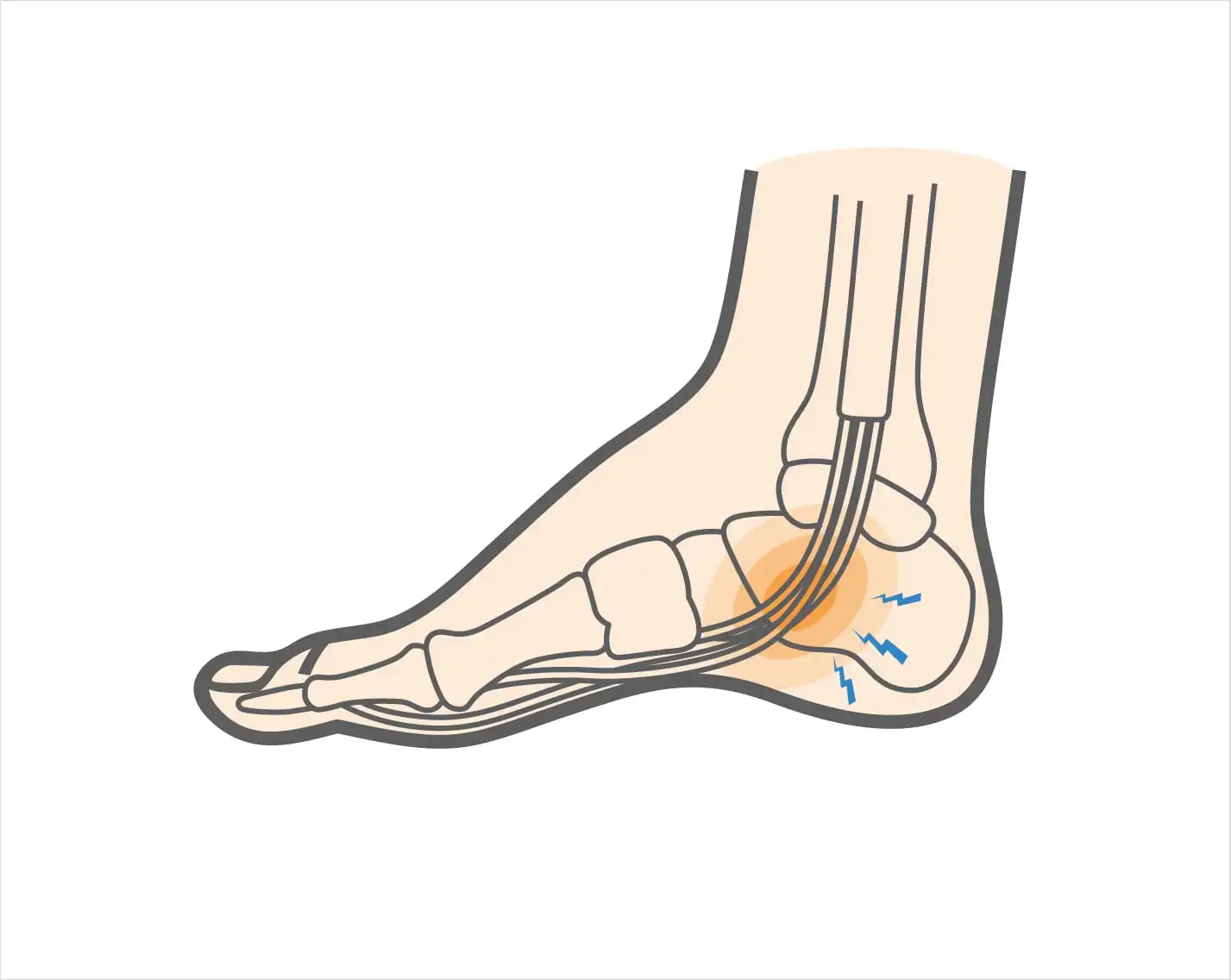
Flexor hallucis longus tendinitis injury is a musculoskeletal condition that affects one of the most important tendons in the foot, the flexor hallucis longus (FHL) tendon. This tendon originates from the lower two-thirds of the fibula, travels down the back of the leg, passes behind the medial malleolus (the bony prominence on the inner ankle), and finally inserts into the base of the distal phalanx of the big toe. The FHL tendon plays a crucial role in foot biomechanics, as it not only flexes the big toe but also stabilizes the medial arch of the foot during walking, running, and jumping. Additionally, it provides essential push-off strength, enabling propulsion during activities that require explosive movements such as sprinting, ballet pointe work, gymnastics, football, and other sports involving repetitive toe-off actions.
When this tendon undergoes excessive stress, repetitive microtrauma, or degenerative changes, it may become inflamed, irritated, or weakened, resulting in a flexor hallucis longus tendinitis injury. This condition is most commonly observed in athletes and individuals who engage in repetitive foot-intensive activities. Dancers, in particular, are prone to this injury, which is often referred to as “dancer’s tendinitis” due to the extreme load placed on the tendon during en pointe and jump maneuvers. Similarly, runners and sportspeople who repeatedly push off the big toe are at higher risk of developing this injury, which can cause pain, swelling, and functional limitations in the foot and ankle.
At DMPhysios, a premier clinic in Noida specializing in spine and sports conditions, the management of flexor hallucis longus tendinitis injury emphasizes patient-centered rehabilitation. Each treatment plan is carefully tailored to the individual’s needs, combining evidence-based physiotherapy techniques, manual therapy, strengthening exercises, and movement retraining. This holistic approach ensures not only the reduction of pain and inflammation but also the restoration of full function, mobility, and long-term tendon health, allowing patients to safely return to their sports and daily activities.
Symptoms
Patients with this injury commonly present with:
- Pain along the inner back of the ankle extending to the big toe.
- Swelling and tenderness along the course of the tendon.
- Pain aggravated by walking, running, jumping, or pushing off the toes.
- A “catching” or “snapping” sensation in severe cases.
- Stiffness in the big toe, especially in the morning or after rest.
- Weakness during push-off phase in walking or sports activity.
- Discomfort during movements requiring ankle plantarflexion (e.g., tiptoe standing).
These symptoms often interfere with daily activities and athletic performance if not treated promptly.
Types of Flexor Hallucis Longus Tendinitis Injury
Though not formally divided into strict types, clinicians describe flexor hallucis longus tendinitis injury in categories based on severity and presentation:
- Acute Tendinitis – Sudden inflammation due to an overuse episode or trauma, leading to sharp pain and swelling.
- Chronic Tendinitis – Long-standing irritation and microtears resulting from repetitive loading, common in professional athletes.
- Stenosing Tenosynovitis – Thickening of the tendon sheath leading to a “triggering” or locking sensation of the big toe.
- Partial or Complete Tear – Severe cases where tendon fibers are disrupted, often requiring prolonged rehab or surgical consultation.
Causes
The main causes include:
- Overuse and repetitive stress (e.g., running, dancing, gymnastics).
- Sudden increase in training intensity or frequency.
- Biomechanical issues such as flat feet or overpronation.
- Improper footwear lacking arch and ankle support.
- Trauma or ankle sprains that overstretch the tendon.
- Muscle imbalances in the calf or intrinsic foot muscles.
- Tight calf muscles (gastrocnemius and soleus) increasing load on the FHL tendon.
Risk Factors
Certain groups are more prone to developing flexor hallucis longus tendinitis injury:
- Ballet dancers (especially en pointe work).
- Sprinters, runners, and jumpers.
- Gymnasts and football players.
- Individuals with poor ankle stability.
- People with flat feet or overpronation.
- Occupations requiring long hours of standing on toes.
- Previous history of ankle injuries.
Awareness of these risk factors helps in early diagnosis and prevention.
Treatment
Management typically begins with conservative approaches:
- Rest and activity modification to reduce tendon overload.
- Ice therapy to reduce swelling and pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) as prescribed.
- Footwear modification with cushioned insoles and arch support.
- Immobilization in severe cases using a walking boot.
- Surgical intervention in rare cases (chronic stenosis or tendon rupture).
However, the cornerstone of recovery lies in physiotherapy rehabilitation, which ensures safe return to activities and long-term tendon health.
Physiotherapy Treatment
At DMPhysios, physiotherapy for flexor hallucis longus tendinitis injury is individualized and patient-centered, focusing on reducing pain, restoring strength, and preventing recurrence. Below is a detailed approach:
1. Pain Management
- Ice packs and cryotherapy.
- Ultrasound or laser therapy for deep tissue healing.
- Manual therapy to reduce soft tissue tightness around the tendon.
2. Range of Motion (ROM) Exercises
- Gentle toe flexion and extension movements.
- Ankle circles to mobilize the joint.
- Big toe towel curls (gripping towel with toes).
3. Stretching Exercises
- Calf stretches (gastrocnemius and soleus) to relieve tension.
- Plantar fascia stretch using a towel or band.
- Toe stretches to gently mobilize the FHL tendon.
4. Strengthening Exercises
- Toe curls with a resistance band.
- Marble pickups with toes to strengthen intrinsic foot muscles.
- Heel raises (progressed to single-leg).
- Eccentric strengthening of the calf and toe flexors to improve tendon resilience.
5. Proprioception and Balance Training
- Single-leg balance on stable and unstable surfaces.
- Bosu ball or wobble board training for ankle control.
6. Gait and Movement Correction
- Analyzing walking and running patterns.
- Correcting overpronation with orthotics.
- Re-educating proper push-off mechanics.
7. Sports-Specific Rehabilitation
- Plyometric drills once pain-free.
- Return-to-sport progression (jumping, sprinting, dancing).
DMPhysios in Noida incorporates all these techniques in a structured rehabilitation protocol, ensuring patients with flexor hallucis longus tendinitis injury not only recover but also return to their sport stronger and safer.
Prevention
Preventing recurrence is just as important as treating the condition. Key preventive measures include:
- Gradual progression of training intensity.
- Regular stretching of calf and foot muscles.
- Strengthening intrinsic foot and ankle stabilizers.
- Wearing supportive footwear with cushioned insoles.
- Cross-training to avoid repetitive overload.
- Addressing biomechanical issues with orthotics or corrective exercises.
- Early management of ankle sprains and foot injuries.
By following these preventive steps, athletes and active individuals can protect themselves against repetitive flexor hallucis longus tendinitis injury.
Conclusion
Flexor hallucis longus tendinitis injury is a debilitating condition that can affect both athletes and active individuals, limiting daily function and sports performance. With proper diagnosis, structured treatment, and comprehensive physiotherapy rehabilitation, recovery is highly successful.
At DMPhysios, a specialized clinic in Noida for spine and sports conditions, the focus is always on patient-centered rehabilitation. By combining manual therapy, targeted exercises, and sports-specific retraining, DMPhysios ensures that patients with flexor hallucis longus tendinitis injury not only recover but also return to their activities stronger, safer, and more confident.
If you are struggling with persistent ankle or big toe pain, don’t let it hold you back. Book a consultation at DMPhysios today and begin your journey toward complete recovery.