Overview
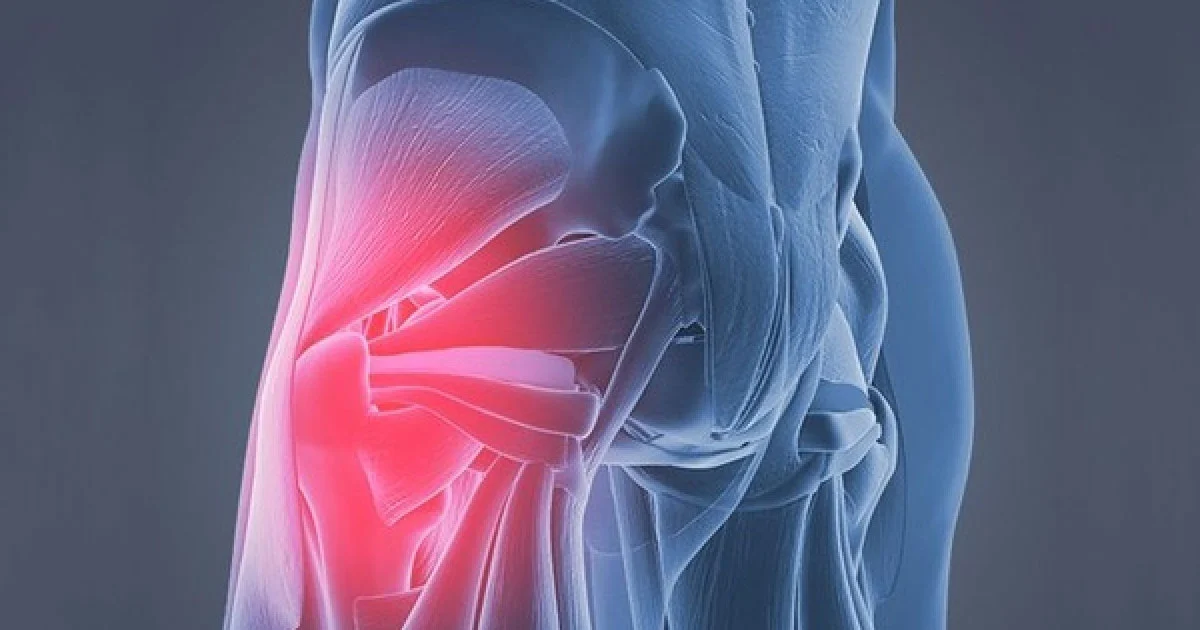
Gluteus medius tendinitis is a condition characterized by irritation or inflammation of the tendon of the gluteus medius muscle, which is situated on the outer aspect of the hip. The gluteus medius plays a vital role in maintaining pelvic stability, especially during movements that require single-leg support, such as walking, running, climbing stairs, or balancing on one leg. When the tendon is subjected to repetitive stress, overuse, sudden trauma, or underlying biomechanical imbalances, it can become inflamed, leading to the development of gluteus medius tendinitis.
This condition often results in pain and discomfort on the outer side of the hip, which can gradually increase and interfere with everyday activities. Simple tasks like standing for extended periods, walking for long distances, or performing exercises may become challenging. If left untreated, gluteus medius tendinitis can progress to chronic pain and contribute to altered gait patterns, hip weakness, or even secondary issues in the lower back or knees due to compensatory movements. Early diagnosis and targeted management are therefore essential for full recovery and to prevent long-term functional limitations.
At DMPhysios, a renowned clinic in Noida specializing in spine and sports-related conditions, patient-centered rehabilitation programs are designed specifically to address gluteus medius tendinitis. Their approach not only focuses on relieving pain but also on restoring strength, improving hip stability, and enabling patients to return safely to their daily routines and athletic activities. With personalized care and evidence-based physiotherapy techniques, DMPhysios helps individuals regain optimal hip function while preventing future recurrences of this common yet debilitating condition.
Symptoms
Patients with gluteus medius tendinitis may experience a variety of symptoms, which typically develop gradually. Key symptoms include:
- Pain on the outer side of the hip, often worsening with activity such as walking, running, or standing on one leg.
- Tenderness when pressing over the greater trochanter (the bony prominence on the side of the hip).
- Weakness in the hip, making it difficult to maintain balance or perform single-leg activities.
- Pain that may radiate down the lateral thigh.
- Discomfort when lying on the affected side, often interfering with sleep.
- Limping or altered gait due to hip pain.
Recognizing these symptoms early can prevent further progression of gluteus medius tendinitis, ensuring timely intervention and rehabilitation.
Types of Gluteus Medius Tendinitis
Although gluteus medius tendinitis is often considered a single condition, clinicians sometimes classify it based on severity:
- Mild Tendinitis
- Involves minor inflammation or micro-tears in the tendon.
- Symptoms may include mild pain and occasional stiffness, usually only during activity.
- Moderate Tendinitis
- Partial tearing of the tendon fibers may occur.
- Patients experience persistent pain, noticeable weakness, and difficulty performing daily activities.
- Severe Tendinitis / Tendinopathy
- Characterized by significant tendon degeneration, partial or complete tears.
- Pain may be constant, with significant functional limitations and risk of secondary hip or lower back problems.
Understanding the type and severity of the condition is critical for developing an effective treatment plan at specialized centers like DMPhysios.
Causes
The development of gluteus medius tendinitis can be attributed to several factors:
- Overuse and repetitive stress: Activities such as running, jumping, cycling, and prolonged standing can strain the gluteus medius tendon.
- Biomechanical imbalances: Weakness in hip or core muscles, leg length discrepancies, or altered gait patterns can increase stress on the tendon.
- Acute trauma: A fall on the hip or a sudden twist of the leg can injure the tendon.
- Degenerative changes: Tendons naturally degenerate with age, making older adults more susceptible to gluteus medius tendinitis.
- Previous hip or back injuries: Injuries affecting the pelvis, sacroiliac joint, or lower back can predispose individuals to tendon irritation.
These factors often combine, causing persistent irritation and inflammation in the gluteus medius tendon.
Risk Factors
Certain individuals are more prone to developing gluteus medius tendinitis:
- Athletes and runners: Frequent repetitive hip movements increase tendon stress.
- Middle-aged adults: Degenerative changes in tendons increase susceptibility.
- People with weak hip muscles: Muscle weakness leads to compensatory overuse of the gluteus medius tendon.
- Obesity: Excess weight increases mechanical load on the hip.
- Post-surgery patients: Hip or lower back surgeries may alter gait mechanics, increasing risk.
Identifying risk factors early allows preventive measures to be implemented, which can significantly reduce the chances of chronic hip pain.
Treatment
Effective management of gluteus medius tendinitis typically involves a combination of rest, pain management, and rehabilitation:
- Rest and activity modification: Avoid activities that aggravate hip pain while maintaining gentle movement to prevent stiffness.
- Pain relief: Non-steroidal anti-inflammatory drugs (NSAIDs) or topical analgesics may help reduce pain and inflammation.
- Ice and heat therapy: Applying ice during acute flare-ups can reduce inflammation, while heat therapy promotes blood flow and healing in later stages.
- Supportive devices: Using orthotics or proper footwear can correct gait imbalances and reduce tendon strain.
While these measures are helpful, physiotherapy remains the cornerstone for long-term recovery.
Physiotherapy Treatment
At DMPhysios, physiotherapy is tailored to each patient, addressing the root cause of gluteus medius tendinitis and promoting full functional recovery. Key physiotherapy interventions include:
1. Pain and Inflammation Management
- Manual therapy: Gentle massage and soft tissue mobilization reduce tendon tension and improve blood flow.
- Ultrasound therapy: Helps decrease inflammation and accelerates tissue healing.
- Accelerated Healing Therapy or heat therapy: Applied in chronic stages to enhance circulation and tendon recovery.
2. Stretching Exercises
- Hip flexor stretch: Helps relieve compensatory tightness that may strain the gluteus medius.
- Piriformis stretch: Reduces tension in surrounding muscles to decrease tendon load.
- Iliotibial band stretch: Prevents excessive lateral pull on the hip.
3. Strengthening Exercises
- Side-lying leg lifts: Targets the gluteus medius directly to rebuild strength.
- Clamshell exercise: Strengthens hip abductors and stabilizers.
- Band walks (lateral and monster walks): Improves dynamic hip stability.
- Bridging exercises: Engages gluteal and core muscles to enhance pelvic control.
4. Neuromuscular Re-education
- Training proper gait and balance helps reduce tendon overload during walking and running.
- Functional exercises mimicking daily activities ensure the tendon adapts to real-world demands.
5. Advanced Rehabilitation
- Progressive resistance training: Gradually increases load on the tendon to restore strength without aggravating inflammation.
- Sports-specific drills: For athletes, tailored programs help safely return to sport while preventing recurrence.
The physiotherapy program at DMPhysios emphasizes patient-centered care, ensuring each plan is customized to the individual’s needs, lifestyle, and goals.
Prevention
Preventing gluteus medius tendinitis is possible with the right strategies:
- Strengthen hip muscles regularly: Incorporate gluteus medius, gluteus maximus, and core strengthening exercises.
- Maintain flexibility: Stretch hip flexors, hamstrings, and IT band to reduce abnormal tension on the tendon.
- Use proper footwear: Shoes that provide support and cushioning reduce mechanical stress.
- Gradual activity progression: Avoid sudden increases in running mileage, weight, or intensity.
- Address gait abnormalities: Orthotics or gait retraining can prevent uneven loading.
Regular physiotherapy check-ups at DMPhysios can help detect early signs of tendon strain and prevent chronic gluteus medius tendinitis.
Conclusion
Gluteus medius tendinitis can significantly impact your quality of life, affecting walking, running, and daily activities. Understanding its causes, symptoms, and risk factors is the first step toward effective management. With the right combination of rest, medical care, and physiotherapy, most individuals can recover fully and prevent recurrence.
At DMPhysios, a clinic located in Noida for spine and sports conditions that provides patient-centered rehabilitation, specialized physiotherapy programs are designed to address the root causes of gluteus medius tendinitis, restore strength, and improve hip function. Whether you are an athlete, a middle-aged adult, or someone experiencing hip pain for the first time, DMPhysios offers expert guidance and structured rehabilitation to help you return to an active, pain-free lifestyle.
If you are experiencing lateral hip pain or suspect gluteus medius tendinitis, reach out to DMPhysios today and take the first step toward effective recovery and long-term hip health.