Understanding Central Sensitization
Article Overview
- The Old View of Pain: Injury = Pain
- The New Understanding: Pain Is an Output of the Brain
- So What Is Central Sensitization?
- How Central Sensitization Develops
- Clinical Clues That Suggest Central Sensitization
- The Neuroscience of a Hypersensitive Nervous System
- Why Pain Without Injury Feels So Real
- Conditions Commonly Associated With Central Sensitization
- How Central Sensitization Is Treated
- The Role of Physiotherapists in Managing Central Sensitization
- The Big Takeaway


P
ain is one of the most misunderstood experiences in human biology. We grow up believing that pain always means damage, a cut means pain, a twisted ankle means pain, a fractured bone means pain. This makes sense… until you meet the patient who wakes up with severe shoulder pain but no injury, or the runner whose knee hurts despite a perfectly normal MRI, or the office worker who develops chronic neck pain without any movement or trauma.
These scenarios raise a simple but important question:
How can someone be in pain when nothing is injured?
This is where the fascinating concept of central sensitization comes in, a phenomenon where the nervous system becomes hypersensitive, amplifying pain signals even when tissues are healthy.
This blog will explore exactly why this happens, how it develops, and what people (and clinicians) can do about it. Written for both patients and professionals, it combines science, real clinical insight, and practical solutions, exactly the kind of patient education resource used and recommended by leading clinics like DMPhysios.
The Old View of Pain: Injury = Pain
For many decades, pain was believed to be a direct signal from injured tissues:
- You cut your finger → pain travels to your brain → you react.
- You twist your ankle → swelling and tissue damage → brain perceives pain.
This “damage-equals-pain” model is appealing because it is simple. But it is also incomplete.
There are countless examples where pain does not match tissue damage:
- Soldiers on the battlefield with severe injuries but no pain.
- People experiencing back pain from “bulging discs” that many healthy people also have without symptoms.
- Athletes who finish a game on a fractured bone before realizing it.
These contradictions forced scientists to rethink pain.
The New Understanding: Pain Is an Output of the Brain
Modern neuroscience shows that:
Pain is not something you feel in your tissues. Pain is something your brain produces to protect you.
This means pain is not a direct measure of damage, it is a measure of perceived threat.
The brain constantly receives information from:
- nerve endings
- immune system
- past experiences
- stress levels
- emotional state
- sleep quality
- muscle tension
- expectations and beliefs
Then it calculates danger.
If your brain believes you need protection, it increases pain.
If it believes you’re safe, it may decrease or eliminate pain, even with injury.
This is why a calm athlete may feel no pain with a broken bone, while a stressed office worker may feel severe pain without any structural abnormality.
So What Is Central Sensitization?
Central sensitization occurs when the brain and spinal cord become overly responsive, causing:
- pain from things that shouldn’t hurt
- increased intensity of normal pain
- pain lasting long after an injury has healed
- spreading of pain to new areas
- extreme sensitivity to pressure, temperature, or movement
Think of it as turning up the “volume knob” on pain.
In a sensitized nervous system:
- minor signals = interpreted as major threats
- normal muscle tension = read as pain
- gentle touch or movement = feels uncomfortable
- stress or fear = increases pain
Importantly:
The issue is not in the tissues. The issue is in how the brain processes information.
This does not mean the pain is “imagined.”
The pain is completely real, the brain has simply become too protective.
Clinics like DMPhysios often see patients who have normal scans and healthy joints but still experience severe pain due to this heightened sensitivity.
How Central Sensitization Develops
Central sensitization rarely appears out of nowhere. It usually builds gradually due to a combination of factors:
a. Persistent or repeated pain
Ongoing pain “trains” the nervous system to become more reactive.
b. Stress, anxiety, depression
These emotional states activate the same brain regions involved in pain perception.
c. Poor sleep and fatigue
Lack of sleep increases inflammatory chemicals in the brain and decreases pain tolerance.
d. Reduced movement
Avoidance reinforces fear → fear increases brain threat → brain outputs more pain.
e. Beliefs and fear
Thoughts like
“Something is seriously wrong,”
“My back is damaged forever,”
“I’m going to make it worse,”
all amplify the brain’s danger response.
f. Past painful experiences
The brain “remembers” pain and becomes hyper-alert.
g. Inflammation
Even low-grade inflammation can sensitize spinal cord neurons.
h. Environmental triggers
Cold weather, loud environments, poor ergonomics, all can amplify pain signals.
Over time, this combination rewires the nervous system, making it more protective than necessary.
Clinical Clues That Suggest Central Sensitization
Not all pain is due to sensitization, but several signs make it likely:
- Pain is disproportionate to the injury
- Pain exists with normal imaging
- Pain spreads beyond the original area
- Symptoms fluctuate with stress or fatigue
- Movement increases pain but does not worsen any tissue
- Multiple sensitive points or tender areas
- Unpredictable pain patterns
- Pain triggered by temperature, light touch, or light pressure
- Pain present for months despite no structural abnormality
Many specialists, including physiotherapists at DMPhysios, use these features to distinguish structural pain from sensitization-driven pain. This helps guide proper rehabilitation.
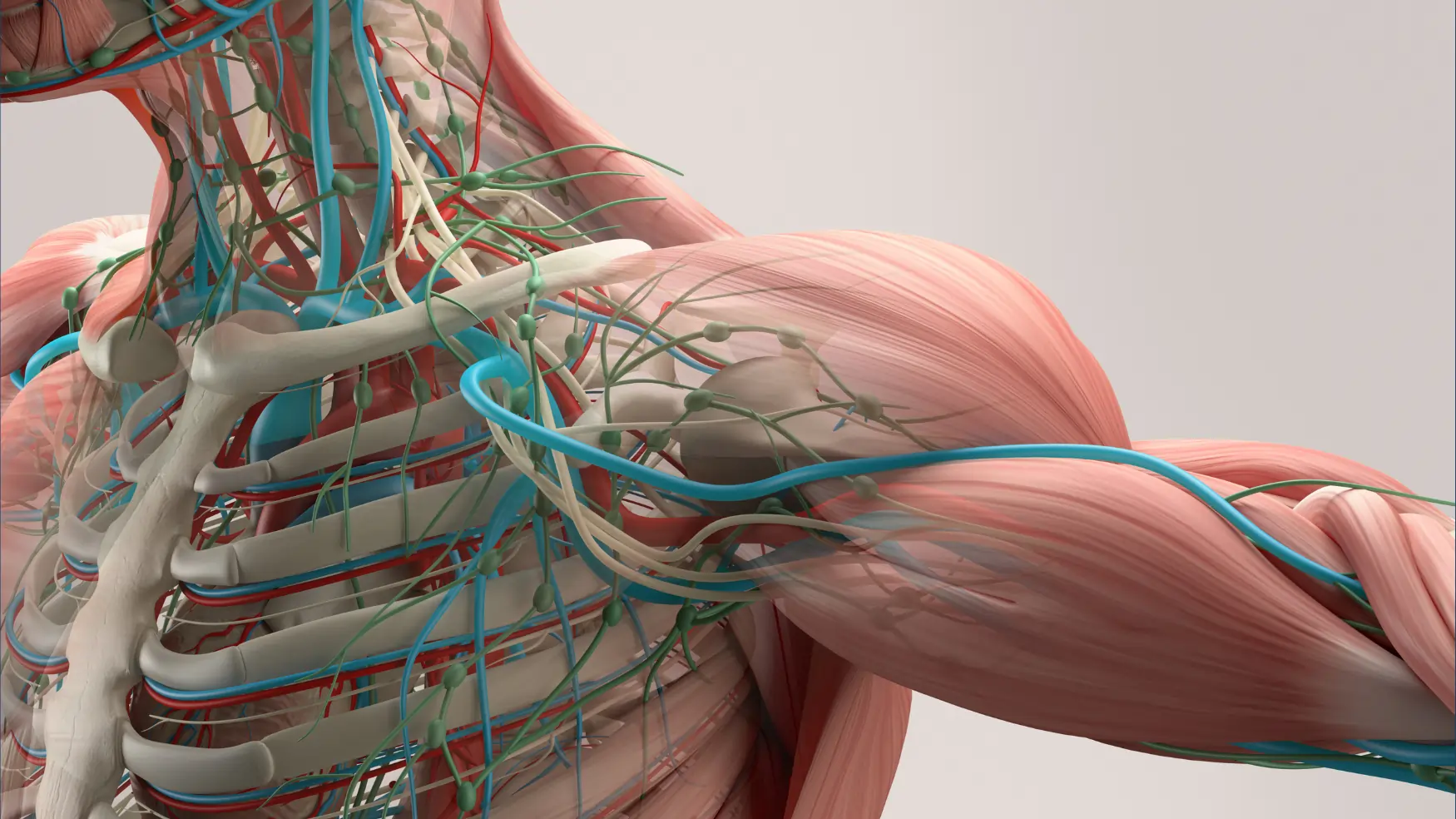
The Neuroscience of a Hypersensitive Nervous System
To understand central sensitization deeply, we must look at what happens inside the spinal cord and brain.
a. Increased excitability of dorsal horn neurons
The spinal cord amplifies incoming messages, like turning up the gain on a microphone.
b. Reduced inhibitory controls
Normally, the brain calms excessive signals.
In sensitization, these controls weaken, letting more pain signals through.
c. Neurochemical changes
Substances like:
- glutamate
- substance P
- cytokines
- bradykinin
- nerve growth factor
all increase, making the system hypersensitive.
d. Structural and functional brain changes
Imaging studies show changes in:
- the amygdala (fear center)
- the prefrontal cortex (decision-making)
- the anterior cingulate cortex (emotional regulation)
- the insula (sensory processing)
Pain becomes deeply linked to emotions, memories, and context.
e. “Pain pathways” become stronger
Just like muscles grow with repetition, neural pathways strengthen when repeatedly used.
The more you experience pain, the more efficient your brain becomes at producing it.
This is why pain with central sensitization can feel severe, constant, and confusing, even when tissues are strong and healthy.
Why Pain Without Injury Feels So Real
Many patients initially resist the idea that sensitization is the cause of their pain.
“Are you saying it’s in my head?”
“Are you saying my pain isn’t real?”
Not at all.
In sensitization, the brain’s protective alarm system misfires, but the alarm is real, loud, and painful.
The brain is not making up pain; it is misinterpreting input.
Consider two examples:
a. Sunburn
Even gentle touch hurts, not because the touch is harmful, but because the nervous system is sensitized.
b. Phantom limb pain
People feel pain in a limb that no longer exists.
No tissue = still pain.
This proves pain can exist independently of tissue damage.
Thus, pain intensity does not always mean injury severity.
The nervous system itself can become the source of pain.
Why Scans Often Show “Nothing”
It’s common for patients to feel frustrated after an MRI or X-ray shows no injury:
- “But I still hurt!”
- “How can nothing be wrong?”
- “Why does my pain feel so severe?”
Imaging shows structure, not function.
You can have:
- normal MRI + severe pain
- abnormal MRI + no pain
- unstable joints + no pain
- healthy joints + hypersensitive nerves
This mismatch is typical in central sensitization.
That is why clinics like DMPhysios focus not only on structural evaluation but also on nervous system behavior and pain science education.
Conditions Commonly Associated With Central Sensitization
While sensitization can occur with any chronic pain condition, it is especially common in:
- Chronic low back pain
- Neck and shoulder pain without injury
- Fibromyalgia
- Chronic tendinopathies
- Tension headaches
- Temporomandibular joint (TMJ) disorders
- Whiplash-associated disorders
- Complex regional pain syndrome
- Persistent post-surgical pain
- Chronic pelvic pain
- Irritable bowel syndrome
- Migraine
- Postural syndromes
- Neuropathic pain conditions
Patients often bounce between specialists without a clear explanation. Once sensitization is identified, treatment becomes much more effective.
How Central Sensitization Is Treated
The good news:
Central sensitization is reversible.
The nervous system can calm down, desensitize, and return to normal functioning.
Effective treatment involves a multi-layered approach:
- Pain Neuroscience Education (PNE)
When patients learn that pain does not always mean injury, fear decreases, movement becomes easier, and sensitivity reduces.
Education alone can create measurable changes in pain and movement.
- Graded Movement & Exercise
Avoiding movement increases sensitivity.
Gentle, progressive movement reduces threat and restores normal brain-body communication.
Key strategies:
- start with comfortable, low-threat movements
- gradually increase intensity
- use pacing instead of pushing
- incorporate mobility, strength, and aerobic exercises
- retrain movement confidence
Clinicians often say,
“Motion is lotion for the nervous system.”
- Aerobic Exercise
Regular aerobic movement:
- boosts natural painkillers (endorphins)
- improves sleep
- reduces systemic inflammation
- enhances mood
- increases circulation
- reduces central excitability
Even 10–15 minutes daily is beneficial.
- Stress Management Techniques
Since stress amplifies pain, techniques like:
- deep breathing
- meditation
- mindfulness
- guided relaxation
- yoga
- gratitude journaling
- nature exposure
help desensitize the nervous system.
- Sleep Optimization
Poor sleep increases inflammatory cytokines and reduces pain tolerance.
Key habits:
- consistent sleep schedule
- limiting screens at night
- cool, dark sleeping environment
- avoiding caffeine in late hours
- gentle evening stretching or relaxing routines
- Graded Exposure to Feared Movements
If someone avoids bending, turning, or lifting:
Avoidance → more fear → more sensitivity → more pain.
Reintroducing movements slowly rebuilds confidence and desensitizes tissues.
- Manual Therapy
Hands-on techniques like:
- soft tissue work
- joint mobilization
- myofascial release
- trigger point therapy
help reduce muscle guarding and allow safe movement.
They do not “fix” the pain generator but reduce the threat level and help the nervous system relax.
Clinics like DMPhysios use these techniques strategically to complement movement-based rehabilitation.
- Cognitive Reframing
Identifying unhelpful thoughts such as:
- “My spine is weak”
- “I’m damaged”
- “Movement is dangerous”
and replacing them with realistic, empowering beliefs reduces fear and dampens sensitization.
- Social Support & Counseling
For long-term sensitization, emotional support plays a major role.
Therapies like CBT, ACT, and mindfulness-based stress reduction have strong evidence.
The Role of Physiotherapists in Managing Central Sensitization
Physiotherapists are uniquely positioned to help because they:
- assess movement fear
- explain pain science
- provide hands-on relief
- give structured exercise programs
- guide graded exposure
- monitor nervous system sensitivity
- build patient confidence
- empower patients with tools, not dependency
A clinic like DMPhysios typically uses:
- detailed assessment
- patient education
- manual therapy
- exercise-based rehab
- posture and ergonomic corrections
- lifestyle modifications
- long-term planning
to help patients overcome pain driven by sensitization.
A Story That Illustrates Central Sensitization
Imagine a house with a smoke alarm.
A normal alarm rings only when there is real smoke.
But a hypersensitive alarm rings when:
- toast is slightly burnt
- shower steam escapes
- someone lights a candle
- dust hits the sensor
There’s no fire, but the alarm is loud and distressing.
Central sensitization is the same.
Your nervous system alarm becomes too sensitive.
It fires off warnings (pain) even when there is no real danger.
The goal of treatment is not to turn the alarm off, pain is still useful.
The goal is to reset the alarm so it only rings when necessary.
Can Central Sensitization Fully Resolve?
Yes.
The nervous system can heal, calm down, and return to normal functioning.
With the right strategies, patients often report:
- reduced pain intensity
- improved confidence
- restored movement
- better sleep
- fewer flare-ups
- higher quality of life
But patience matters.
Desensitization is like training a muscle or learning a new skill.
Consistency → rewiring → recovery.
The Big Takeaway
Pain does not always equal injury.
Sometimes pain reflects a highly protective, highly sensitive nervous system that is doing its best to defend you.
The solution is not rest, pills, or fear.
The solution is:
- understanding pain
- moving in safe, progressive ways
- managing stress
- building strength
- improving sleep
- reframing beliefs
- desensitizing the nervous system
Clinics like DMPhysios guide patients through this process every day, helping people reclaim their lives even when pain seems confusing, persistent, or overwhelming.
Pain is real.
Your experience is valid.
And most importantly, your nervous system can change.
You can recover, rebuild, and return to a pain-free, confident life.