Myofascial Pain Is the New Epidemic
Why Trigger Points Are Behind Most Aches Today
Article Overview
- What exactly is myofascial pain and what are trigger points?
- Why the sudden attention? Three converging trends
- How Trigger Points Form: A Practical, Evidence-based Model
- Common Clinical Presentations
- What The Science Says About Treatments
- Putting it together: A Practical, Evidence-based Treatment Pathway
- Case Vignette
- Practical Advice For Patients
- Future Directions: Where Research Is Heading


E
verywhere you look, clinics, fitness studios, social media reels, and GP waiting rooms, people are talking about “muscle knots,” “trigger points,” and aching regions that move around or return no matter how much you stretch.
That chatter isn’t just a trend: mounting clinical evidence and new research into fascia, muscle physiology, and pain processing have pushed myofascial pain into the spotlight as a major, often under-recognized driver of chronic musculoskeletal symptoms. This article unpacks the biology, the evidence, and the practical roadmap clinicians (and curious patients) can use to identify and treat myofascial pain. Along the way I’ll explain why trigger points matter more than ever and how clinics like DMPhysios are adapting patient-centered care to this modern epidemic.
What exactly is myofascial pain and what are trigger points?
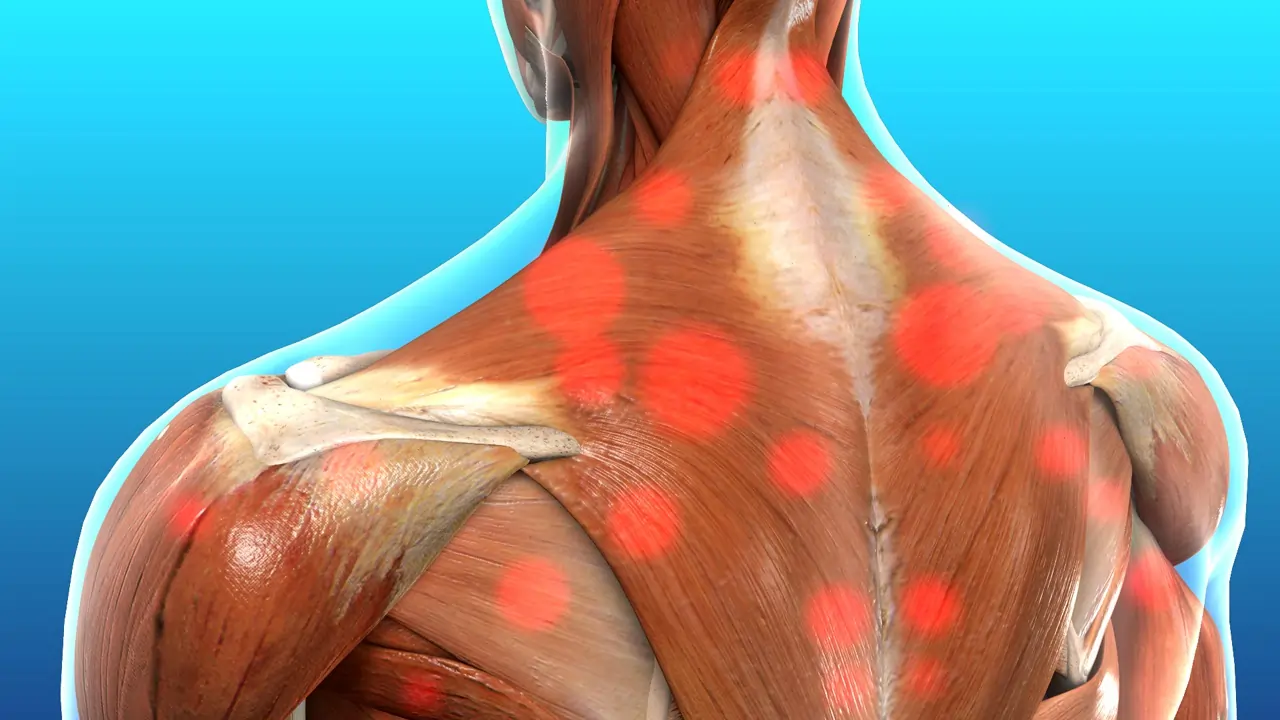
Myofascial pain syndrome (MPS) is a chronic regional pain condition associated with taut bands of skeletal muscle and myofascial trigger points (MTrPs), small, hyperirritable nodules in muscle that are exquisitely tender and can refer pain to distant areas when pressed. Trigger points are commonly described as “muscle knots,” but clinically they are defined by a cluster of signs: a palpable tight band, a focal tender spot, a local twitch response on palpation, and a reproducible referred pain pattern. These phenomena make MPS clinically distinct from joint or neuropathic pain and explain why patients often report pain that migrates or seems “mismatched” to imaging findings. Large contemporary reviews and consensus statements have clarified these diagnostic features, helping clinicians distinguish MPS from other causes of chronic pain.
Why the sudden attention? Three converging trends
- Prevalence and clinical burden. Myofascial trigger points are highly prevalent in people with common musculoskeletal complaints, for example, studies show a high rate of trigger points in patients with non-specific low back and neck pain and in many with chronic headaches. That prevalence translates directly to clinical workload: many people seeking care for “back pain” or “tension headaches” have a myofascial component that needs specific treatment.
- Better research and clearer definitions. Over the last decade researchers have refined definitions, mapped referral patterns, and conducted methodical reviews of treatments like manual therapy, dry needling, and myofascial release. This improved evidence base has pushed MPS out of the “hands-on folklore” bucket and into mainstream musculoskeletal medicine.
- New understanding of fascia and neurophysiology. Fascia, the connective tissue web around muscles, is not just packing material. Recent work shows fascia contains contractile cells, sensory nerve endings, and plays a role in force transmission, proprioception, and pain modulation. This has encouraged clinicians to treat the whole myofascial system rather than isolated muscles.
How Trigger Points Form: A Practical, Evidence-based Model
Trigger points don’t appear out of nowhere. Current research suggests a multifactorial model:
- Local muscle overload or microtrauma (from repetitive postures, sudden strain, or overuse) can produce local ischemia and metabolic disturbance.
- Excessive muscle fiber contraction, a dysfunctional motor endplate and increased acetylcholine release can create a tight band and pain.
- Local biochemical changes (elevated inflammatory mediators and nociceptive substances) sensitize local and central pain pathways.
- Fascial changes (adhesions or altered glide) and central sensitization (increased responsiveness of spinal/brain circuits) then amplify and perpetuate the cycle.
This integrated view, muscle contracture, local biochemical irritation, fascial restriction, and central nervous system involvement, explains why a single treatment rarely “cures” long-standing myofascial pain and why multimodal care is most effective.
Common Clinical Presentations
Patients with myofascial pain often report:
- Aching that moves or refers to other regions (e.g., a shoulder trigger point creating pain down the arm).
- Pains that flare with certain postures or repetitive tasks (desk work, phone use, repetitive lifting).
- Stiffness, limited range, and focal tight bands that feel like knots.
- Pain disproportionate to imaging findings, MRI may show degenerative changes unrelated to the current pain.
- Associated symptoms such as headache, decreased sleep quality, and regional weakness.
Clinicians will find trigger points by careful palpation, reproducing the patient’s pain or referred pattern, and observing a local twitch response in some cases. Given the prevalence of trigger points in common complaints, most assessment pathways now include a myofascial screen.
What The Science Says About Treatments
No single treatment is a silver bullet, but modern studies suggest several interventions can meaningfully reduce pain and improve function when used as part of a multimodal plan.
Manual Therapies And Myofascial Release
Hands-on techniques (ischemic compression, deep friction, myofascial release) show benefit for short-term pain relief and improving range. Trials vary in quality, but systematic reviews support their role as part of a larger program that includes exercise and education.
Dry Needling And Trigger Point Injection
Dry needling, inserting a fine needle into the trigger point to elicit a twitch response, has accumulated the strongest evidence for short- to mid-term pain reduction in several regions (neck, shoulder, low back) and for improving pressure pain thresholds. Systematic reviews and meta-analyses, including analyses up to 2023, support moderate effectiveness compared with sham or no treatment, though the magnitude and duration of benefit vary by condition and technique. Wet needling (trigger point injection with a local anesthetic) also shows benefit in some settings.
Exercise And Motor Control Retraining
Exercise aimed at motor control, strength, and graded loading is critical. Targeted strengthening and movement retraining reduce re-injury risk, restore normal muscle coordination, and reduce recurrence of trigger points. Importantly, exercise reduces central sensitization when progressed appropriately.
Adjuncts: Education, Sleep, Stress Management
Because stress, poor sleep, and psychosocial factors can perpetuate pain, therapies that address sleep hygiene, pacing, and stress management are essential for long-term outcomes. Patient education that explains referred pain and the myofascial model reduces fear and improves adherence.
Putting it together: A Practical, Evidence-based Treatment Pathway
- Assessment & Screening. Look for taut bands, tender nodules, referral patterns and reproduce symptoms with palpation. Rule out red flags and neuropathic pain. DMPhysios’ clinicians routinely include a myofascial screen in new musculoskeletal assessments to avoid missed diagnoses.
- Short-term Symptom Control. Use targeted manual therapy, ischemic compression, and when appropriate, dry needling or trigger point injection to reduce acute pain and break the protective muscle guarding. Short-term objective: reduce pain enough to engage in exercise. Many clinics (including DMPhysios) combine dry needling with a supervised strengthening plan for faster recovery.
- Rehabilitation & Motor Control. Progress to graded loading, postural correction, and movement retraining. Focus on endurance of stabilizers, reciprocal inhibition of overactive muscles, and restoring fascial glide where indicated.
- Lifestyle & Central Modulation. Address sleep, work ergonomics, stress, and activity pacing. Cognitive reassurance and education about referred pain reduce catastrophizing and improve outcomes.
- Prevention & Maintenance. Teach self-treatment (self-compression, foam rolling, targeted mobility drills), maintain conditioning, and schedule periodic follow-ups. Clinics like DMPhysios offer short maintenance programs for people prone to recurring trigger points.
Case Vignette
A 38-year office worker presents with 6 months of neck pain, frequent tension headaches, and a constant “knot” at the base of the right skull. Cervical imaging shows minimal degenerative change at C5–C6 that doesn’t match her pain. A focused myofascial assessment reveals a taut band in the right upper trapezius with a trigger point that reproduces her headache referral pattern when pressed. Treatment includes two sessions of dry needling and ischemic compression over two weeks, combined with a 6-week program of scapular motor control and postural re-education. Her headache frequency drops by 70% and neck pain becomes manageable, illustrating how identifying and treating MTrPs within a multimodal plan provides rapid, meaningful change.
What About Controversial Claims And Limits Of The Evidence?
There remain controversies. The exact biological nature of trigger points is still debated, and not all studies find large, long-lasting effects from single interventions. Placebo and contextual effects are real contributors to pain relief and should be harnessed ethically. Importantly, while dry needling shows consistent short-term benefit, its long-term superiority over exercise-based programs is less clear, so clinicians should avoid over-reliance on any single therapy. Recent comprehensive reviews urge clinicians to use evidence-based combinations of manual therapy, needling (when skilled and indicated), and progressive exercise for best outcomes.
Practical Advice For Patients
Don’t ignore the “knot.” If a focal tight band reproduces your pain, consider a clinical myofascial assessment. Early treatment often prevents chronicity. DMPhysios recommends early screening for anyone with persistent regional pain lasting more than a few weeks.
- Move, but progress gradually. Gentle, targeted exercise reduces recurrence. Avoid aggressive stretching of painful tissue, it can sometimes increase irritation.
- Sleep and stress matter. Improve sleep hygiene and use relaxation techniques; both reduce pain sensitivity.
- Try self-care tools. Foam rollers, massage balls, and targeted compression can relieve acute tightness; learn correct techniques from a physiotherapist to avoid harm.
- Seek multimodal care. Combine manual therapies, needling if appropriate, and a progressive exercise plan for lasting benefit. DMPhysios’ programs blend these elements with education and ergonomic advice.
How Modern Clinics Are Adapting: The DMPhysios a Approach
At DMPhysios we’ve seen a steady rise in patients whose primary or contributory diagnosis is myofascial pain. In response, DMPhysios has refined assessment templates to include trigger point mapping and developed integrated care pathways combining: hands-on myofascial release, graded exercise, dry needling by credentialed clinicians, and patient education. The team emphasizes functional outcomes (return to work, sleep improvement, and activity tolerance) rather than imaging findings. DMPhysios also tracks outcomes so therapies evolve with the evidence — a model that other clinics are beginning to copy. If you’re wondering about practical options, DMPhysios recommends an initial focused assessment plus a 4–6 session trial combining manual therapy and guided exercise to see early gains.
(Those seeking more on dry needling or myofascial release should ask clinicians about training, consent, and expected timelines; skilled application matters.)
Future Directions: Where Research Is Heading
Research today focuses on clarifying trigger point histopathology, mapping referred pain mechanisms, and optimizing combined treatment regimens. We’re also seeing sophisticated investigations into how fascia behaves as a sensory and motor organ, and how that behavior contributes to chronic regional pain. Improved clinical trials with larger samples and standardized outcome measures are emerging, which will help refine guidelines and identify which patients benefit most from specific interventions. Expect more precise clinical pathways in the next 3–5 years as evidence consolidates.
Key Takeaways
- Myofascial pain and trigger points are a major, under-recognized driver of many chronic aches and headaches.
- Trigger points are real clinical entities with reproducible signs and referral patterns; accurate diagnosis matters.
- Multimodal care – Manual therapy, dry needling (when appropriate), exercise, and education, gives the best outcomes.
- Fascia is more than scaffolding: it’s an active tissue involved in pain and movement, and that insight is reshaping treatment.
- Clinics that combine assessment, evidence-based interventions, and patient education (like DMPhysios) are best placed to manage the modern myofascial epidemic.
Here’s an extended, polished Call to Action (CTA) version that flows naturally, sounds professional, and fits perfectly at the end of your blog:
Ready To Take The Next Step?
If you’re dealing with recurring neck pain, stubborn shoulder tightness, low back discomfort, or headaches that just won’t go away, it may be more than “just stress”, trigger points and myofascial dysfunction could be the real cause. The good news is that these issues are highly treatable when approached correctly.
Look for a clinician who will:
- Screen thoroughly for myofascial trigger points (MTrPs).
- Explain your pain in clear, simple terms so you truly understand what’s happening in your body.
- Offer a short, evidence-based treatment plan combining manual therapy, dry needling when appropriate, and progressive rehabilitation.
- Teach you self-management strategies so you can maintain long-lasting relief, not just temporary comfort.
At DMPhysios, our team specializes in exactly this kind of comprehensive, patient-centered care. We combine expert assessment with hands-on myofascial techniques, targeted dry needling, and structured strengthening programs to help you break the pain cycle, safely, effectively, and without creating dependency on passive treatments.
If you’re ready to understand your pain, treat its root cause, and finally get back to the activities you love.
Book your assessment at DMPhysios today. Your recovery starts with one step, and we’re here to guide you through every part of it.